-
Fish and Prostate Cancer Risk: Fact or Fiction
By William Faloon, Luke Huber, ND, MBA, Kira Schmid, ND, Blake Gossard, Scott Fogle, ND
Several scientific studies have found a reduction in prostate cancer associated with increased omega-3 intake.1-11 A recent report purportedly showed the opposite.12
This report was based on a single blood test of plasma fatty acids in a group of 834 men who were followed up to six years to assess prostate cancer risk (low- and high-grade disease). A smaller group of 75 men was followed up to nine years to assess only high-grade prostate cancer risk.
The results showed that slightly higher omega-3 plasma percentages from this single blood test were associated with a greater risk of low-grade ( 44% ) and high-grade ( 71% ) prostate cancers over the multi-year follow-up.
This report was turned into news stories with headlines blaring “ Omega-3 fatty acids may raise prostate cancer risk . ”
Omitted from the media frenzy was the fact that this study was not about fish oil supplement users. The authors admitted they did not know how the study participants achieved what turned out to be very low omega-3 plasma percentages in all groups.
In fact, omega-3 plasma levels were only about 40% of what would be expected in health conscious people taking the proper dose of fish oil .12 ,13 The insufficient levels of plasma omega-3s in all the study subjects were overlooked by the media. Had these very low plasma levels of omega-3s been recognized, it would have been apparent that this report had no meaning for those who boost their omega-3 consumption through diet and supplements.
Also absent from the reporting was that more men with slightly higher omega-3 plasma levels had confounding risk factors for greater risk of contracting prostate cancer at baseline, such as having higher PSA scores and a positive family history . Although the authors attempted to statistically control (through a statistical model called multivariate analysis) for some of these risk factors in their analysis, the concern remains that the baseline data was confounded and therefore the statistical analysis invalid , and that the reported results are compromised by higher rates of preexisting disease along with a genetic predisposition , not because of the miniscule variance in the amount of their plasma omega-3 .
Prostate cancer sharply increases by 120% to 180% in men who have a first-degree relative who had contracted prostate cancer. Nearly double the men who contracted prostate cancer in this study had a positive family history, and although the researchers attempted to statistically control for this confounding factor, this fact was conveniently overlooked by the mainstream media as omega-3s were instead labeled the culprit.
Associating a one-time plasma omega-3 reading with long term prostate cancer risk is ludicrous. That’s because plasma omega-3 changes rapidly with short-term dietary changes. It does not reflect long-term incorporation of omega-3 into cells and tissues. In this report, differences in baseline omega-3 blood measures were so trivial that if a man had just one salmon meal the night before, he could have wound up in the “higher” omega-3 group even if he never ingested another omega-3 again.14
Numerous flaws in this report render its findings useless for those who supplement with purified fish oils and follow healthy dietary patterns. This article represents Life Extension®’s initial rebuttal to this spurious attack on omega-3s that was blown out of proportion by the media.
Prostate cancer is a slow developing malignancy that can take decades to manifest as clinically-relevant disease. Commonly recognized risk factors for contracting prostate cancer are diet, body mass, race, family history, hormone status, and age.15,16
An under-recognized risk factor associated with developing prostate cancer is coronary artery disease .17 We at Life Extension long ago observed that men with clogged coronary arteries often developed prostate cancer (and vice versa). A renowned prostate oncologist named Stephen Strum, M.D., made a similar observation and established a common factor behind coronary heart disease and prostate cancer, i.e., bone loss .
Coronary artery disease is clearly linked with osteoporosis ,18 as lack of vitamin K prevents calcium from binding to bone and instead allows it to infiltrate and harden the arteries . The ensuing bone loss results in the excessive release of bone-derived growth factors that fuel prostate cancer propagation and metastasis.
Long after Dr. Strum published his elaborate correlation, a 2012 study of 6,729 men showed coronary artery disease to be associated with a 35% increased risk of prostate cancer .17
The reason we bring up the connection of heart disease and prostate cancer is that the authors of the controversial study apparently failed to assess overall baseline health status of the study subjects. We initially suspected that men in the higher group of plasma omega-3 (which turned out to be low by our standards) were more likely to have coronary heart disease. That’s because men with heart disease are told by their cardiologists to eat less red meat and more cold-water fish. So it would not be surprising if the plasma percentage of omega-3 was higher in men with prostate cancer as they may have been trying to eat healthier to avoid bypass surgery or a sudden heart attack.
When we asked the authors of the report if they assessed the baseline cardiovascular status of the subjects, their reply was, “ No, I don’t believe this to be the case. ”
Family History Predisposition
If your father or brother develops prostate cancer, your odds of getting it are about 120% to 180% greater than if you don’t have this family history.19
In the report attacking omega-3s, men who contracted prostate cancer had almost double the proportion of first-degree relatives with a history of prostate cancer compared with controls. Although the study authors apparently attempted to control for this baseline risk factor through the use of statistical modeling of selected variables (multivariate analysis), this confounding factor calls into question much of this report’s negative findings, but was not even mentioned in the media’s rush to create headline grabbers.
Men with a family history of prostate cancer often have witnessed the long term death spiral that prostate cancer patients suffer through. As a result, they attempt to adapt healthier lifestyles to avoid becoming a victim of their hereditary genes.
Since eating well-done red meat has long been associated with increased prostate cancer risk, men with unfavorable family histories are more likely to include at least some cold-water fish in their diets, and therefore have higher omega-3 percentage plasma levels. This does not mean the marginally higher omega-3 caused their prostate cancer.
This is partially corroborated with the data from the study participants who did not develop prostate cancer, but had higher plasma percentage levels of pro-inflammatory omega-6 fats. This indicated these individuals had little concern about what they ate since they had about half the family history rate of prostate cancer.
Fortunately there may be ways to alter family history genetic predispositions for prostate cancer by eating lots of cruciferous vegetables , maintaining youthful hormone balance , ensuring optimal vitamin D status, and taking compounds that favorably alter gene expression like metformin and curcumin .20-28
Baseline PSA Higher in Those Who Contracted Prostate Cancer
Prostate specific antigen (PSA) is a blood marker of prostate disease.
Standard laboratory reference ranges often allow PSA to reach 4.0 ng/mL before flagging a potential problem. A more progressive view of the PSA is that any number over 2.4 ng/mL should be viewed with suspicion, with a digital rectal exam performed and a follow-up PSA blood test done in three months.
Life Extension has published comprehensive articles about how to properly interpret PSA results, but to state it succinctly: Aging men with PSA readings greater than 2.4 ng/mL are at higher risk for developing clinically relevant prostate cancer and should initiate aggressive steps to reverse the underlying process.
In the report that associated higher omega-3 blood levels with increased prostate cancer incidence, 41.1% of the men who went on to develop prostate cancer had baseline PSA readings greater than 3.0 ng/mL. In the group that did not develop prostate cancer, only 7.3% has a PSA baseline reading greater than 3.0 ng/mL.
Although the study researchers attempted to statistically control for other confounding factors in their analysis like family history, age, and education level, this PSA finding implies that many of the men who developed prostate cancer already had it ( pre-existing disease ) when the baseline plasma omega-3 level was measured. This finding of 5.6 times more men who developed prostate cancer with a baseline PSA level greater than 3.0 ng/mL compared to the “no cancer” group is impossible to rationally discount. To reiterate, below is the data on the baseline PSA readings from the report the media used to discredit omega-3s:
- 7.3% of the “No Cancer” group had PSA of ≥3.0
- 41.1% of the “Total Cancer” group had PSA of ≥3.0
This critical piece of data was ignored in the tabloid-like media articles that erroneously blamed the increase in prostate cancer on omega-3s.
Study Subjects do not Appear to Have Taken Fish Oil Supplements
Life Extension scientists repeatedly reached out to the authors of the negative report, but did not receive a response as to whether any attempt was made to ascertain the source of the omega-3 in the study subjects’ blood. We wanted to know if these men regularly ate cold-water fish or took at least some fish oil supplements.
Despite our requests, no clarification was made available by study authors as to the level of dietary supplementation with fish oil, and if so, the source of fish oil used in the study.
Based upon the very low plasma percentage levels of omega-3 fatty acids detected in the study, the implication is that dietary supplementation with fish oil likely did not occur. Instead, based upon the low levels of omega-3 plasma phospholipids detected, the source appears to have been primarily (potentially exclusively) diet only. As we will show soon, it appears that none of the men in this study consumed much in the way of cold-water fish either.
Omega-3 Levels Were Low in All Study Subjects
You will be shocked to learn how low the average plasma percentages of omega-3 were in all these study subjects, whether they were in the high or low rate of prostate cancer group.
Plasma phospholipid testing for fatty acids was used in this study. However, this type of fatty acid testing can vary widely depending upon short-term dietary intake. In contrast, long-term uptake by cells and tissues of the body is far less dependent upon short-term changes in diet. For this reason, erythrocyte (red blood cell) fatty acid indices are far better at evaluating cellular uptake over time as a result of fish ingestion and fish oil supplementation.
For example, data indicates that supplementing with about 2 grams of omega-3 fatty acids from fish oil leads to an increase in erythrocyte (red blood cell) omega-3 fatty acid percentage from about 4% at baseline to about 8% at eight weeks.13
In a case analysis conducted by Life Extension staff, a healthy diet that included fish but not fish oil supplementation resulted in an omega-3 red blood cell (RBC) equivalence level of 6.06% .
However, a standard diet supplemented with 3.6 grams of EPA/DHA from purified fish oil resulted in an omega-3 RBC equivalence level of 10.59% . Thus, compared to what can be achieved with a healthy diet alone, adding a high quality fish oil supplement can nearly double a person’s omega-3 RBC equivalence score, which is consistent with the published literature.
Therefore, if participants in the report alleging an association with fish and prostate cancer had been taking meaningful doses of fish oil supplements, their levels should have been substantially higher than what the study authors reported. Instead, for men in the prostate cancer group of this study, the percentage of plasma long-chain omega-3 fatty acids was only 4.66% … a lower level than historic baselines taking no supplemental omega-3s.13
The numbers below should clarify this glaring flaw that renders conclusions from this report claiming fish or fish oil increases prostate cancer utterly meaningless:
- Omega-3 RBC equivalence percentage of a moderate fish eater: 6.06%
- Omega-3 RBC equivalence percentage when taking 3.6 grams/day EPA/DHA: 10.59%
- Average long-chain omega-3 plasma percentage in study group with higher prostate cancer rates: 4.66%
- Average long-chain omega-3 plasma percentage in study control group (no prostate cancer): 4.48%
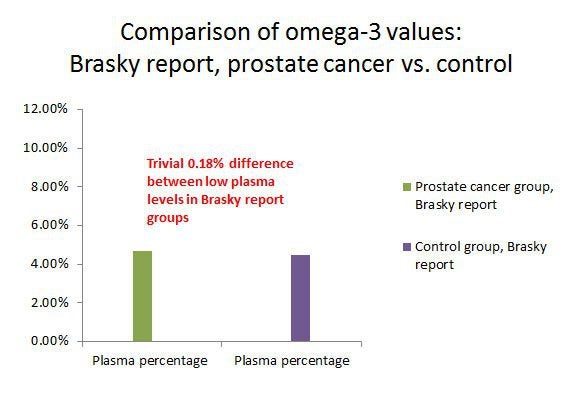 Figure 1: If you can’t see a difference in the two bars showing plasma percentage of omega-3s between men who contracted prostate cancer and those who did not, that’s because there is virtually no difference. The 0.18% variation could have resulted from men eating just a few ounces of fish the night before their one-time baseline blood draw. These low percentages of plasma omega-3s indicate these men were not taking fish oil supplements, nor were they eating much in the way of omega-3-rich foods in their diet.
Figure 1: If you can’t see a difference in the two bars showing plasma percentage of omega-3s between men who contracted prostate cancer and those who did not, that’s because there is virtually no difference. The 0.18% variation could have resulted from men eating just a few ounces of fish the night before their one-time baseline blood draw. These low percentages of plasma omega-3s indicate these men were not taking fish oil supplements, nor were they eating much in the way of omega-3-rich foods in their diet.There may be no need to provide any more rebuttal than the numbers posted above. They make it clear that the average subject in their groups were consuming very little cold-water fish and certainly no meaningful fish oil supplement. Their entire study population was so negligible in omega-3 that no relevant correlation can be drawn for health conscious people today choosing omega-3-rich foods (like cold-water fish) and high-potency fish oil supplements.
Yet based on this study of men who consumed relatively no omega-3s, frenzied news reporters were advising the public to stop eating cold-water fish and avoid omega-3 supplements.
Virtually No Difference in Omega-3 in Men Who Developed Prostate Cancer
When reading the frantic news reports, you would have thought the omega-3 difference in men with up to 71% increased risk of prostate cancer must have been huge .
At Life Extension , our very first reaction was that the researchers were comparing cardiac patients who gobbled down huge amounts of fish oil supplements to normal individuals who consume relatively little omega-3s. Our initial assumption was that since heart disease patients have higher prostate cancer rates, then that would explain why higher omega-3 could be mistakenly associated with increased prostate cancer risk, since heart disease patients are known to consistently take high-potencies of omega-3s through diet and supplements. How wrong our early conjecture was!
It turns out that the differences in omega-3 plasma phospholipid levels between groups were slight. In fact they were so close that we at Life Extension would classify them all as being too narrow to extrapolate meaningful data.
Our goal is to get the red blood cell (RBC) omega-3 index values in Life Extension members to 8%-11% as this level was shown to offer the greatest protection against sudden myocardial infarction, yet the average quartile for plasma long-chain omega-3 fatty acids in the prostate cancer cases in the report associating fish oil with prostate cancer was only 4.66% .
Now look how narrow the difference is between men with higher prostate cancer rates. In the group whose average baseline blood draw showed 4.48% plasma long-chain omega-3 fatty acids, there was no increased prostate cancer risk. But if the omega-3 percentage average went up to 4.66% (about 1/5 of one percent), prostate cancer rates skyrocketed, according to the report’s authors.
We’re talking here of a difference of 0.18% in the percentage of plasma omega-3 fatty acids that supposedly caused a 43% to 71% increase in prostate cancer incidence. Dedicated fish oil supplement users, on the other hand have over 100% higher omega-3 levels than seen in this study of men who apparently consumed little cold-water fish and no omega-3 supplements.
To put this into real-world perspective, the trivial difference ( 0.18% ) in plasma omega-3 between men with no prostate cancer and those with prostate cancer could occur if a man ate just a few ounces of a cold-water fish like salmon the night before.
Remember, plasma phospholipid testing for fatty acids was used in this study. However, this type of fatty acid testing can vary widely depending upon short-term dietary intake. In contrast, long-term uptake by cells and tissues of the body is far less dependent upon short-term changes in diet. For this reason, the omega-3 RBC equivalence score is far better at evaluating cellular uptake over time as a result of fish ingestion and fish oil supplementation.
There was only one baseline blood draw. The men were followed up to six years (low-grade and high-grade cancer), with a smaller group followed up to nine years to see who would get high-grade prostate cancer. Those who developed prostate cancer were then compared against their baseline blood draw done years earlier.
This kind of methodology is open to misinterpretation and errors even if there were large variances in omega-3 fatty acid percentages, but the 0.18% difference is so tiny that it has no relevance to aging humans who choose to include omega-3-rich foods in their diet and supplement with fish oil.
This may be the first study that seeks to discredit a food/supplement (i.e., omega-3s), where the human subjects were not even taking a fish oil supplement nor ingesting significant amounts of an omega-3 food.
A 0.18% difference in plasma omega-3 fatty acids between men who contracted prostate cancer and those who did not is infinitesimally small. To extrapolate a conclusion from this very small difference that eating fish or taking fish oil supplements is risky, false, misleading, and meaningless … but it did generate a lot of news headlines.
Life Extension is concerned that some men will decrease consumption of omega-3s resulting in a devastating increase of their triglycerides, thrombotic, inflammatory and atherogenic risks. An epidemic of coronary artery blockage and ischemic stroke will soon follow.
Results Are Completely Inconsistent With the Known Biology, Pathophysiology, and Biochemistry of Prostate Cancer
A fundamental aspect of quality research is consistency, and repeatability.
Stated another way, for a medical finding to be considered valid, the results should not contradict well-established facts involving known biology, physiology, biochemistry, etc. Furthermore, the finding should be repeatable by other scientists.
The report attacking omega-3s is inconsistent with a variety of aspects of the well-established scientific and medical literature.
For example, upon close inspection of the data (and not simply a top-line, parroted response by the mainstream media eager to generate headlines), non-smokers had more aggressive prostate cancer, and non-drinkers (alcohol) had higher risk of prostate cancer, and prostate cancer case subjects were less likely to report a history of diabetes than controls.
Based upon these results, the implication is that men who wish to avoid prostate cancer should consume excess calories and develop diabetes, drink alcohol heavily, and abuse tobacco.
This is completely inconsistent with well-established science, and utter nonsense.
In fact, numerous scientific studies show fish oil omega-3 fatty acids offer significant protective benefit for prostate health.
Fish Oil Omega-3 Fatty Acids Offer the First Line of Defense Against Prostate Cancer
In contrast to this attack on omega-3s, the scientific literature overwhelmingly identifies diets high in omega-6 fats, trans -fatty acids, and saturated fats as associated with greater prostate cancer risk, whereas increased intake of long-chain omega-3 fats from fish has been shown to reduce risk. Based on consistent findings across a wide range of human populations, scientific research has identified why eating the wrong kinds of fatty acids provokes a stimulatory effect on prostate cancer.29,30
To ascertain what occurs after dietary fatty acids are consumed, the biochemical pathway for fatty acid metabolism provides the answers. For example, let us assume that for dinner, you eat a steak (a source of saturated fat, as well as arachidonic acid) and a salad, along with a typical salad dressing rich in linoleic acid, an omega-6 fat (e.g., safflower oil).
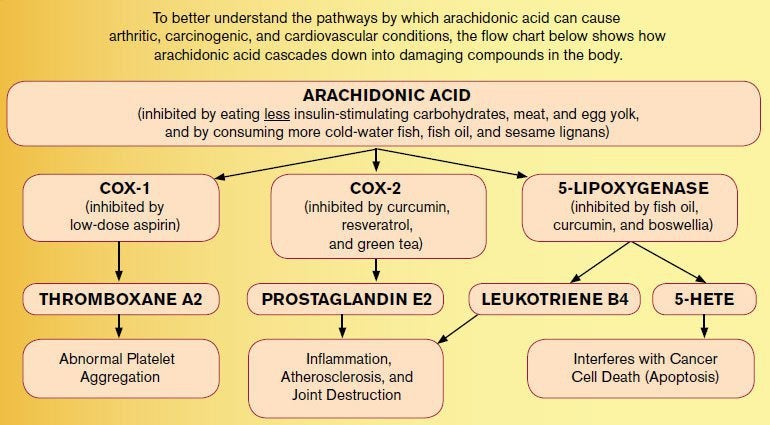
Biochemically, saturated fat and linoleic acid, a type of omega-6 fat, readily convert to arachidonic acid in the body. In response, the body attempts to compensate for excess arachidonic acid through the 5-lipoxygenase (5-LOX) pathway. Multiple studies strongly show that 5-LOX enzymatic by-products like leukotriene B4 and 5-HETE directly stimulate prostate cancer cell proliferation through several well-defined mechanisms.31-36
For example, arachidonic acid is metabolized by 5-LOX to 5-hydroxyeicosatetraenoic acid (5-HETE), a potent survival factor that prostate cancer cells use to escapedestruction.37,38 Consuming a diet of foods rich in arachidonic acid, or precursors to arachidonic acid like the omega-6 fat linoleic acid, directly provokes the production of dangerous 5-LOX metabolic by-products, which can promote the progression of prostate cancer. In addition to 5-HETE, 5-LOX also metabolizes arachidonic acid into leukotriene B4, a potent pro-inflammatory agent that causes destructive reactions throughout the body and inflicts severe damage to the arterial wall.39-41
If arachidonic acid levels are reduced, a corresponding suppression of the 5-LOX products 5-HETE and leukotriene B4 will occur. A wealth of scientific research clearly demonstrates that supplementation with long-chain fatty acids like EPA and DHA from fish oil can help reduce the production of arachidonic acid-derived eicosanoids in the body.42
In contrast with the misinterpreted results presented in this report of men who were not consuming significant amounts of omega-3s, many other clinical studies indicate substantial benefit with omega-3 fatty acid intake in prostate cancer.
Additional Studies Indicate Substantial Benefit With Increased Intake of Omega-3 Fatty Acids
The report attacking omega-3s conflicts with prior studies demonstrating that increased intake of omega-3 fats has been shown to reduce prostate cancer risk and diets high in omega-6 fats are associated with greater risk. The analysis also suggests a relationship between increased omega-6 fatty acid levels and decreased risk of prostate cancer, which is, again, utterly inconsistent with the known pro-inflammatory effects of omega-6 fatty acids.
- A 2010 meta-analysis found a 63% reduction in prostate cancer death rates in those with higher fish consumption.1
- A 2004 study of 47 ,866 men found a trend toward decreased risk of prostate cancer with increasing levels of EPA and DHA.2
- A 2007 Harvard study of 14, 916 men found lower incidence of prostate cancer in men who had higher levels of long chain omega-3 fatty acids.3
- A 2013 Harvard study of 293, 464 men found increased omega-3 fatty acid intake was associated with significantly lower rate of fatal prostate cancer.4
- A 2012 Harvard study of 525 men found a 40% lower prostate cancer death rate among men with the highest intake of marine fatty acids.5
- A 2011 Duke University study found an increased omega-6:omega-3 ratio (i.e., more omega-6 and less omega-3) was associated with a significantly elevated risk of high grade prostate cancer.6
- A 1999 New Zealand study found significantly lower rates of prostate cancer with higher blood levels of EPA and DHA.7
- A 1999 Korean study found increased blood levels of omega-3 fatty acids associated with lower rates of prostate cancer and benign prostatic hyperplasia.8
- A 2003 prospective study reported “that men with high consumption of fish had a lower risk of prostate cancer, especially for metastatic cancer.”10
- A 2010 study that evaluated nutrient intake and prostate cancer risk concluded “High intake of omega-6 fatty acids, through their effects on inflammation and oxidative stress, may increase prostate cancer risk.”43
- The University of Chicago conducted a study published in 2004 that showed PSA levels rose in tandem with the omega-6 to omega-3 ratio in Jamaican men whose PSA was >10 ng/mL. The researchers noted “Increased levels of Omega6 PUFAs and the ratio of Omega6/Omega3 PUFAs in Jamaican men are associated with an increased mean PSA level and risk of prostate cancer.”44
- In addition to the clinical trial literature indicating consistent benefits with omega-3 fatty acid intake, traditional Japanese and Mediterranean diets rich in omega-3 fatty acids show a strong, consistent risk reduction in prostate cancer vs. Western diets rich in omega-6 and saturated fat.
Traditional Diets in Japan and The Mediterranean Region High in Fish are Protective Against Prostate Cancer
The results set forth by authors of the negative report on fish oil that omega-3 intake may be linked to prostate cancer are inconsistent, and in abject contrast, to longstanding evidence that diets high in marine lipids, such as the traditional Japanese diet and the Mediterranean diet, are protective against prostate cancer.
For example, the traditional Japanese diet, rich in omega-3 fatty acids from fish, confers protection against prostate cancer, as does the relatively high intake of fermented soy products and relatively low levels of saturated fat.45 The characteristics of the traditional Japanese diet high in soybean products, high in fish, and low in red meat are highly relevant in prostate cancer biology. In all likelihood, the traditional Japanese diet reduces the risk of prostate cancer through a combination of characteristics that generate a synergistic, anti-cancer effect (on prostate cancer).
Likewise, the protective properties of the Mediterranean diet in relation to heart disease and prostate cancer risk are well-established. Several aspects of this dietary pattern are protective, including regular consumption of small fish (smaller fish are less likely to contain contaminants than larger predatory fish such as tuna), high olive oil intake (there is synergy between olive polyphenols and fish oil), high daily ingestion of fresh vegetables, whole fruits (not pasteurized fruit juice rich in concentrated fructose), high-fiber cereals and legumes, and low intake of saturated animal fats and red meat.46
Benefit Clearly Outweighs Risk for Fish Oil Supplementation Among Men
Overwhelming evidence currently available strongly favors fish oil supplementation for most aging humans.
Fish oil and greater marine omega-3 intake have repeatedly and consistently been shown to reduce cardiovascular risk across multiple types of studies. For example:
A randomized, placebo-controlled trial found 1,800 mg of combined EPA plus DHA was associated with a 10% lower rate of cardiac events, 12% lower rate of non-fatal infarctions, and an almost 11% lower rate of cardiac deaths.47
In a large intervention study, 18,000 patients were randomized to receive either a statin medication alone or a statin plus 1,800 mg of EPA-fish oil daily. After five years, those with a history of coronary artery disease had a 19% lower rate of major coronary events in the statin-plus EPA-fish oil group compared to the statin-only group.48
A randomized, double-blind, placebo-controlled trial with chronic hemodialysis patients found that 1,700 mg of omega-3 fatty acids daily was associated with a 70% reduction in the relative risk of myocardial infarction.49
A randomized, controlled trial using 3,300 mg of EPA and DHA (and then a decreased dosage) found a trend toward lower cardiovascular event occurrence with fish oil supplementation. Seven cardiovascular events occurred in the placebo group (not given fish oil) while only two cardiovascular events occurred in the fish oil-supplemented group during the study.50
A meta-analysis with an average fish oil dose of 3,700 mg found lowered systolic blood pressure by an average 2.1 mmHg and diastolic by 1.6 mmHg .51
In a randomized trial with peripheral arterial disease patients, 2,000 mg of omega-3 fatty acids daily resulted in a 49% improvement in flow-mediated dilation, a marker of endothelial cell health.52
The GISSI-Prevenzione study (a large, randomized, controlled trial) found that 1,000 mg/day of EPA and DHA in 11,323 patients with a history of recent myocardial infarction reduced the risk of total mortality by 20% and sudden death by 45% .53,54
The DART study — a randomized, controlled trial that examined the effects of advising 2,033 subjects to increase dietary fatty fish — revealed a 29% reduction in all-cause mortality compared with those not advised.55
A 2009 meta-analysis of randomized, controlled trials found that dietary supplementation with omega-3 fatty acids reduced the incidence of sudden cardiac death in subjects with prior myocardial infarction.56
Another 2009 meta-analysis of randomized, controlled trials found that dietary supplementation with omega-3 fatty acids reduced the risk of cardiovascular death, sudden cardiac death, all-cause mortality, and non-fatal cardiovascular events in patients with a history of certain cardiovascular events or risk factors.57
A 2008 meta-analysis found a significant reduction in death from cardiac causes with fish oil supplementation.58
A 2002 meta-analysis of randomized, controlled trials concluded that omega-3 fatty acids reduced overall mortality, mortality due to myocardial infarction, and sudden death in patients with coronary heart disease.59
Will this Flawed Report Prompt an Epidemic of Prostate Cancer?
Regrettably, the public is poorly served by relying on a sound-bite frenzied news media for health data, which often involves parading a provocative medical headline without a deep, thorough evaluation of the study’s validity.
This “science by ambush” denies an opportunity for meaningful rebuttal, since the media never wants to admit last week’s headline news story was bogus.
The average percentage difference ( 0.18% ) of plasma long-chain omega-3 fatty acids from a single baseline test renders this study meaningless. The authors don’t even know if their study subjects were eating fish or taking fish oil supplements. We at Life Extension have criticized certain studies that solely rely on food questionnaires, but this attack on omega-3s didn’t even attempt to ascertain if study subjects were ingesting the nutrient (omega-3s) in question. Yet its authors presumptuously warn of potential risks in consuming supplemental omega-3s!
The lack of rigor, as well as multiple layers of methodological problems and errors, notwithstanding the complete lack of consistency with the known, well-established biology and biochemistry of prostate cancer should prompt outrage in the scientific and medical community.
The danger of this deeply flawed, compromised analysis is that aging men obtaining health information through the mainstream media will cease omega-3 fatty acid ingestion.
The consequences may be profound if aging men shun omega-3 fatty acid supplementation as a result of this flawed study and follows its implied recommendations to consume more omega-6 fats, which enhance inflammation and create a better environment for prostate cancer, as well as cardiovascular disease to flourish.
Although the researchers attempted to statistically model (through multivariate analysis) and control for some (but not all) critical, confounding risk factors like family history, the higher baseline PSA readings (implying more preexisting cancers) and positive family history (1st degree male relative with prostate cancer) in men who went on to develop prostate cancer raise concerns for the integrity of the analysis results. Along with these confounding factors, the marginal difference in baseline plasma omega-3 levels of men who later developed prostate cancer cannot rationally implicate omega-3s as having a causal or causative effect. The plasma omega-3 levels of the entire study group showed consumption of omega-3 from food was inadequate and intake of meaningful fish oil supplementation non-existent.
Educated health consumers should continue to ingest omega-3 fatty acids.
This report will be updated as more of Life Extension ’s scientific advisors provide their input.
References
- Szymanski KM, Wheeler DC, Mucci LA. Fish consumption and prostate cancer risk: a review and meta-analysis. The American journal of clinical nutrition. Nov 2010;92(5):1223-1233.
- Leitzmann MF, Stampfer MJ, Michaud DS, et al. Dietary intake of n-3 and n-6 fatty acids and the risk of prostate cancer. The American journal of clinical nutrition. Jul 2004;80(1):204-216.
- Chavarro JE, Stampfer MJ, Li H, Campos H, Kurth T, Ma J. A prospective study of polyunsaturated fatty acid levels in blood and prostate cancer risk. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. Jul 2007;16(7):1364-1370.
- Bosire C, Stampfer MJ, Subar AF, et al. Index-based dietary patterns and the risk of prostate cancer in the NIH-AARP diet and health study. American journal of epidemiology. Mar 15 2013;177(6):504-513.
- Epstein MM, Kasperzyk JL, Mucci LA, et al. Dietary fatty acid intake and prostate cancer survival in Orebro County, Sweden. American journal of epidemiology. Aug 1 2012;176(3):240-252.
- Williams CD, Whitley BM, Hoyo C, et al. A high ratio of dietary n-6/n-3 polyunsaturated fatty acids is associated with increased risk of prostate cancer. Nutrition research (New York, N.Y.). Jan 2011;31(1):1-8.
- Norrish AE, Skeaff CM, Arribas GL, Sharpe SJ, Jackson RT. Prostate cancer risk and consumption of fish oils: a dietary biomarker-based case-control study. British journal of cancer. Dec 1999;81(7):1238-1242.
- Yang YJ, Lee SH, Hong SJ, Chung BC. Comparison of fatty acid profiles in the serum of patients with prostate cancer and benign prostatic hyperplasia. Clinical biochemistry. Aug 1999;32(6):405-409.
- Astorg P. Dietary N-6 and N-3 polyunsaturated fatty acids and prostate cancer risk: a review of epidemiological and experimental evidence. Cancer causes & control : CCC. May 2004;15(4):367-386.
- Augustsson K, Michaud DS, Rimm EB, et al. A prospective study of intake of fish and marine fatty acids and prostate cancer. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. Jan 2003;12(1):64-67.
- Aronson WJ, Kobayashi N, Barnard RJ, et al. Phase II prospective randomized trial of a low-fat diet with fish oil supplementation in men undergoing radical prostatectomy. Cancer prevention research (Philadelphia, Pa.). Dec 2011;4(12):2062-2071.
- Brasky TM, Darke AK, Song X, et al. Plasma Phospholipid Fatty Acids and Prostate Cancer Risk in the SELECT Trial. Journal of the National Cancer Institute. Jul 10 2013.
- Cao J, Schwichtenberg KA, Hanson NQ, Tsai MY. Incorporation and clearance of omega-3 fatty acids in erythrocyte membranes and plasma phospholipids. Clinical chemistry. Dec 2006;52(12):2265-2272.
- Harris W. et al. Comparative effects of an acute dose of fish oil on omega-3 fatty acid levels in red blood cells versus plasma: Implications for clinical utility. Journal of Clinical Lipidology, 5/9/2013.
- American Cancer Society. Available at: http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-risk-factors . Accessed 7/15/2013.
- University of Maryland Medical Center. Prostate cancer. Available at: http://umm.edu/health/medical/altmed/condition/prostate-cancer Accessed 7/15/2013.
- Thomas JA, 2nd, Gerber L, Banez LL, et al. Prostate cancer risk in men with baseline history of coronary artery disease: results from the REDUCE Study. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. Apr 2012;21(4):576-581.
- Farhat G. et al. The link between osteoporosis and cardiovascular disease. Clin Cases Miner Bone Metab. 2008 Jan-Apr; 5(1): 19–34.
- Bruner DW, Moore D, Parlanti A, Dorgan J, Engstrom P. Relative risk of prostate cancer for men with affected relatives: systematic review and meta-analysis. International journal of cancer. Journal international du cancer. Dec 10 2003;107(5):797-803.
- Chinni SR, Li Y, Upadhyay S, Koppolu PK, Sarkar FH. Indole-3-carbinol (I3C) induced cell growth inhibition, G1 cell cycle arrest and apoptosis in prostate cancer cells. Oncogene. May 24 2001;20(23):2927-2936.
- Cohen JH, Kristal AR, Stanford JL. Fruit and vegetable intakes and prostate cancer risk. Journal of the National Cancer Institute. Jan 5 2000;92(1):61-68.
- Morgentaler A. Testosterone For Life. New York, NY: McGraw-Hill; 2008.
- Vijayakumar S, Mehta RR, Boerner PS, Packianathan S, Mehta RG. Clinical trials involving vitamin D analogs in prostate cancer. Cancer journal (Sudbury, Mass.). Sep-Oct 2005;11(5):362-373.
- Lou YR, Qiao S, Talonpoika R, Syvala H, Tuohimaa P. The role of Vitamin D3 metabolism in prostate cancer. The Journal of steroid biochemistry and molecular biology. Nov 2004;92(4):317-325.
- John EM, Schwartz GG, Koo J, Van Den Berg D, Ingles SA. Sun exposure, vitamin D receptor gene polymorphisms, and risk of advanced prostate cancer. Cancer research. Jun 15 2005;65(12):5470-5479.
- Ben Sahra I, Laurent K, Giuliano S, et al. Targeting cancer cell metabolism: the combination of metformin and 2-deoxyglucose induces p53-dependent apoptosis in prostate cancer cells. Cancer research. Mar 15 2010;70(6):2465-2475.
- Teiten MH, Gaascht F, Eifes S, Dicato M, Diederich M. Chemopreventive potential of curcumin in prostate cancer. Genes & nutrition. Mar 2010;5(1):61-74.
- Piantino CB, Salvadori FA, Ayres PP, et al. An evaluation of the anti-neoplastic activity of curcumin in prostate cancer cell lines. International braz j urol : official journal of the Brazilian Society of Urology. May-Jun 2009;35(3):354-360; discussion 361.
- Newcomer LM, King IB, Wicklund KG, Stanford JL. The association of fatty acids with prostate cancer risk. The Prostate. Jun 1 2001;47(4):262-268.
- Niclis C, Diaz Mdel P, Eynard AR, Roman MD, La Vecchia C. Dietary habits and prostate cancer prevention: a review of observational studies by focusing on South America. Nutrition and cancer. 2012;64(1):23-33.
- Hassan S, Carraway RE. Involvement of arachidonic acid metabolism and EGF receptor in neurotensin-induced prostate cancer PC3 cell growth. Regulatory peptides. Jan 15 2006;133(1-3):105-114.
- Moretti RM, Montagnani Marelli M, Sala A, Motta M, Limonta P. Activation of the orphan nuclear receptor RORalpha counteracts the proliferative effect of fatty acids on prostate cancer cells: crucial role of 5-lipoxygenase. International journal of cancer. Journal international du cancer. Oct 20 2004;112(1):87-93.
- Matsuyama M, Yoshimura R, Mitsuhashi M, et al. Expression of lipoxygenase in human prostate cancer and growth reduction by its inhibitors. International journal of oncology. Apr 2004;24(4):821-827.
- Gupta S, Srivastava M, Ahmad N, Sakamoto K, Bostwick DG, Mukhtar H. Lipoxygenase-5 is overexpressed in prostate adenocarcinoma. Cancer. Feb 15 2001;91(4):737-743.
- Ghosh J, Myers CE. Arachidonic acid stimulates prostate cancer cell growth: critical role of 5-lipoxygenase. Biochemical and biophysical research communications. Jun 18 1997;235(2):418-423.
- Gao X, Grignon DJ, Chbihi T, et al. Elevated 12-lipoxygenase mRNA expression correlates with advanced stage and poor differentiation of human prostate cancer. Urology. Aug 1995;46(2):227-237.
- Sundaram S, Ghosh J. Expression of 5-oxoETE receptor in prostate cancer cells: critical role in survival. Biochemical and biophysical research communications. Jan 6 2006;339(1):93-98.
- Myers CE, Ghosh J. Lipoxygenase inhibition in prostate cancer. European urology. 1999;35(5-6):395-398.
- Helgadottir A, Manolescu A, Thorleifsson G, et al. The gene encoding 5-lipoxygenase activating protein confers risk of myocardial infarction and stroke. Nature genetics. Mar 2004;36(3):233-239.
- Poff CD, Balazy M. Drugs that target lipoxygenases and leukotrienes as emerging therapies for asthma and cancer. Current drug targets. Inflammation and allergy. Mar 2004;3(1):19-33.
- Crooks SW, Bayley DL, Hill SL, Stockley RA. Bronchial inflammation in acute bacterial exacerbations of chronic bronchitis: the role of leukotriene B4. The European respiratory journal. Feb 2000;15(2):274-280.
- Adam O, Beringer C, Kless T, et al. Anti-inflammatory effects of a low arachidonic acid diet and fish oil in patients with rheumatoid arthritis. Rheumatology international. Jan 2003;23(1):27-36.
- Kristal AR, Arnold KB, Neuhouser ML, et al. Diet, supplement use, and prostate cancer risk: results from the prostate cancer prevention trial. American journal of epidemiology. Sep 1 2010;172(5):566-577.
- Ritch CR, Brendler CB, Wan RL, Pickett KE, Sokoloff MH. Relationship of erythrocyte membrane polyunsaturated fatty acids and prostate-specific antigen levels in Jamaican men. BJU international. Jun 2004;93(9):1211-1215.
- Mori M, Masumori N, Fukuta F, et al. Traditional Japanese diet and prostate cancer. Molecular nutrition & food research. Feb 2009;53(2):191-200.
- Ferris-Tortajada J, Berbel-Tornero O, Garcia-Castell J, Ortega-Garcia JA, Lopez-Andreu JA. [Dietetic factors associated with prostate cancer: protective effects of Mediterranean diet]. Actas urologicas espanolas. Apr 2012;36(4):239-245.
- Singh RB, Niaz MA, Sharma JP, Kumar R, Rastogi V, Moshiri M. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival–4. Cardiovascular drugs and therapy / sponsored by the International Society of Cardiovascular Pharmacotherapy. Jul 1997;11(3):485-491.
- Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. Mar 31 2007;369(9567):1090-1098.
- Svensson M, Schmidt EB, Jorgensen KA, Christensen JH. N-3 fatty acids as secondary prevention against cardiovascular events in patients who undergo chronic hemodialysis: a randomized, placebo-controlled intervention trial. Clinical journal of the American Society of Nephrology : CJASN. Jul 2006;1(4):780-786.
- von Schacky C, Angerer P, Kothny W, Theisen K, Mudra H. The effect of dietary omega-3 fatty acids on coronary atherosclerosis. A randomized, double-blind, placebo-controlled trial. Annals of internal medicine. Apr 6 1999;130(7):554-562.
- Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. Journal of hypertension. Aug 2002;20(8):1493-1499.
- Schiano V, Laurenzano E, Brevetti G, et al. Omega-3 polyunsaturated fatty acid in peripheral arterial disease: effect on lipid pattern, disease severity, inflammation profile, and endothelial function. Clinical nutrition (Edinburgh, Scotland). Apr 2008;27(2):241-247.
- Marchioli R, Barzi F, Bomba E, et al. Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI)-Prevenzione. Circulation. Apr 23 2002;105(16):1897-1903.
- Efficacy of n-3 polyunsaturated fatty acids and feasibility of optimizing preventive strategies in patients at high cardiovascular risk: rationale, design and baseline characteristics of the Rischio and Prevenzione study, a large randomised trial in general practice. Trials. 2010;11:68.
- Burr ML, Fehily AM, Gilbert JF, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. Sep 30 1989;2(8666):757-761.
- Zhao YT, Chen Q, Sun YX, et al. Prevention of sudden cardiac death with omega-3 fatty acids in patients with coronary heart disease: a meta-analysis of randomized controlled trials. Annals of medicine. 2009;41(4):301-310.
- Marik PE, Varon J. Omega-3 dietary supplements and the risk of cardiovascular events: a systematic review. Clinical cardiology. Jul 2009;32(7):365-372.
- Leon H, Shibata MC, Sivakumaran S, Dorgan M, Chatterley T, Tsuyuki RT. Effect of fish oil on arrhythmias and mortality: systematic review. BMJ (Clinical research ed.). 2008;337:a2931.
- Bucher HC, Hengstler P, Schindler C, Meier G. N-3 polyunsaturated fatty acids in coronary heart disease: a meta-analysis of randomized controlled trials. The American journal of medicine. Mar 2002;112(4):298-304.
-
Libido, Testosterone and Nutrition
Dr Cecilia Tregear explains why she believes that sexual activity is a great tool for gauging health and what you can do to give your score a boost.
Forget Botox. If you want to look and feel young, then what you should really be doing is swinging from the chandeliers.
Regular sex in your youth, your middle years and beyond is the ultimate elixir of youth, says hormone and anti-ageing specialist Dr Cecilia Tregear.
World-renowned Dr Tregear, who is based at the Wimpole Skin Clinic in Harley Street, London, has worked with hundreds of couples over the course of her 25-year career.
‘I began to notice a pattern,’ she says. ‘The couples who were having lots of regular sex almost always looked younger than those who weren’t. They were also slimmer, fitter, healthier and happier.’
‘Sexual activity, in my view, is an accurate thermometer for measuring health.’
But far too many of us aren’t having great sex. Or much, if any, of it. Either we’re too tired, have lost our libidos or have got stuck in a rut or boring routine which makes sex with our partner about as appealing as doing the laundry. We feel unattractive — and as a result, we aren’t as attracted to our partner either.
A poor sex life can be caused by hormonal problems as a result of a thyroid condition, or the effects of the menopause/ andropause (male menopause) which deplete sex hormones.
But lifestyle factors, such as eating poorly, smoking, drinking too much alcohol, stress and lack of exercise, can also have a massive impact on sexual health.
Dr Tregear realised the people who were having lots of sex in their relationships had one key factor in common: their diet. All of them were eating extremely nutritious food.
She explains: ‘Good nutrition is essential for the healthy production of hormones which maintain the libido and allow for regular and fulfilling sexual activity.”
She has devised the Between the Sheets diet, which promises to perk up your libido. Combined with regular exercise (and, if necessary, supplements containing natural hormones) it should ensure you not only have regular, great sex — just like you did in your youth — but look and feel younger too …
Step One: Feed Your Brain
According to Dr Tregear, the first step to boosting your love life is to feed your brain. ‘The biggest sexual organ is the brain, which produces the chemicals and hormones that trigger feelings of love and attraction, arousal and orgasm,’ she says. ‘We need to make sure we’re eating the right foods to ensure the production of these chemicals and hormones.’
First, it’s important to have a diet that boosts the levels of the neurotransmitter dopamine, released by the brain. Dopamine is the feel-good chemical associated with the emotions of anticipation and desire. As such, it is vital to a healthy sex drive.
Boosting levels in the brain has been shown to be incredibly successful at treating flagging libidos, and there are currently dopamine drugs on trial. However, you won’t need them if you eat well.
Dopamine-boosting food: To boost levels it’s essential to eat lots of proteins, because these contain amino acids, which are converted into neurotransmitters in the brain.
Amino acids are found in red meat, oily fish, eggs, cottage cheese, beans, peas, milk, wheatgerm, beetroot and bananas.
The production of dopamine also relies on vitamins and minerals, so make sure you eat plenty of fresh fruit and vegetables — watermelon, which contains vitamins A, B6 and C, is a particularly good addition to the diet.
The following spices can also boost dopamine levels: basil, black pepper, cayenne pepper, chilli peppers, cumin, fennel, flax seeds, garlic, ginger, mustard seeds, rosemary, sesame seeds, tarragon and turmeric.
Drinking a small amount of alcohol can also boost dopamine, which is why a glass of wine can help to put you in the mood.
Step Two: Balance Your Hormones
Having a good balance of hormones is essential to a healthy sex life, which is why the menopause — when hormone levels drop — can cause havoc with your sex life. There are three hormones responsible for arousal and sexual desire: oestrogens, which are present in both men and women, testosterone , also in both men and women, and DHEA (dehydroepiandrosterone), which is found in women only.
‘A good balance of animal fat in meat and fish and good cholesterol, found in eggs for example, encourages the production of sex hormones, improving libido,’ says Dr Tregear. ‘It’s vital to eat plenty of good quality protein, ideally a portion with every meal,’.
Oestrogens: Avoid excessive amounts of fibre (such as brown bread) which lower oestrogen by stopping its absorption. Having cereal and toast for breakfast is the worst thing you can do for your hormones. Scrambled egg with salmon is a much better option.
Avoid alcohol, too. Anything more than the odd glass of wine with dinner, once or twice a week, has a detrimental effect on hormones, impairing both oestrogen and testosterone production.
Research also shows that smoking reduces levels of oestrogen in the body.
Testosterone : Essential for sex drive in both men and women. The reason that oysters are an aphrodisiac is because they are high in zinc, which is necessary for the production of testosterone.
Other foods high in zinc include meat, eggs, seafood and tofu. Avoid coffee or other high-caffeine drinks. Caffeine de-activates testosterone, which will reduce your libido.
DHEA: This vital hormone is made in the adrenal glands and levels usually peak around the age of 25. Although the libido-promoting effects of DHEA are less well publicised than other hormones such as oestrogen, doctors are now reporting that increasing levels can have dramatic effect on libido.
To boost your levels of DHEA you need to increase the amount of ‘good fats’ in your diet by eating more oily fish, such as salmon and anchovies, and also green leafy vegetables such as spinach, rocket and watercress.
The adrenal glands, which produce hormones including DHEA, are also the part of the body that respond to stress.
Excess stress can cause the adrenals to produce stress hormones at the expense of sex hormones. Spices and salty food make the adrenal glands work more efficiently to produce more DHEA.
Step Three: Boost Your Energy
For good sex, you need stamina and energy. While a generally healthy diet will help you feel strong and healthy, it’s important to eat food that will increase your levels of Human Growth Hormone (HGH). This hormone increases sexual desire and provides the stamina and energy needed for a sexual marathon. To increase production, eat organic protein from beef, fish, and chicken.
Root vegetables such as carrots and parsnips can also help, as can low-sugar fruits, such as blueberries.
Avoid pulses and cereals and refined sugars, which can cause your energy to peak and then slump.
Thyroid hormones help us to maintain energy. To work, the thyroid needs iodine, which is found in kelp, seaweed, oysters, clams and tuna.
Finally, vitamin B also plays a major role in energy production, as it helps convert carbohydrates into sugar to fuel the body’s energy.Foods rich in this include avocados, duck, lamb, sweet potatoes and sunflower seeds.
While it can be tempting to get an energy boost by eating sugar and sweets, this is a mistake, because it will cause short-lived energy peaks followed by a longer dip in energy. And that’s not what your partner will be looking for in the bedroom!
Boston Testosterone is a Testosterone Replacement , Wellness and Preventative Medicine Medical Center that treats and prevents the signs and symptoms associated with Andropause and hormone imbalances. With affiliates nationally, Boston Testosterone offers hormone replacement therapy, weight loss protocols, erectile dysfunction (ED), Sermorelin-GHRP2 therapy and neutraceutical injectable therapies for men and women. Their medical facilities offer physician examinations and treatment programs that incorporate the latest in medical science.
Originally Published by dailymail.co.uk
“The Greatest Health of Your Life” ℠
Boston Testosterone Partners
www.facebook.com/BostonTestosterone
855.617.MEDS (6337)/781-269-5953
cblaisdell@corenewengland.com
-
Testosterone Therapy is associated with reduction in pain in men
New studies have associated a reduction in pain in men undergoing testosterone replacement therapy. The results were presented at The Endocrine Society’s 95th Annual Meeting in San Francisco.
“In this study, we attempted to determine whether testosterone replacement improves pain perception and tolerance, and quality of life in men with low testosterone levels due to narcotic analgesics,” said the study’s lead author Shehzad Basaria, MD, Medical Director, Section of Men’s Health, Aging, & Metabolism at Brigham & Women’s Hospital, Harvard Medical School, in Boston, MA. “We found that testosterone administration in these men was associated with a greater reduction in several measures of pain sensitivity during laboratory pain testing compared with men who were on placebo.”
In addition to being highly addictive, opioid use is associated with a number of side effects, including suppression of the hypothalamic-pituitary-gonadal axis in both women and men, resulting in decreased testosterone production. Low testosterone, in turn, can result in sexual dysfunction, decreased muscle mass, increased fat mass and decreased quality of life.
Previous animal research has demonstrated that castration of rodents is associated with increased pain perception while testosterone replacement reduces pain perception, suggesting an analgesic effect of this sex steroid. Whether these beneficial effects can be replicated in humans, however, remained unclear.
In this study, investigators found that, compared to placebo, testosterone therapy significantly improved pain perception and tolerance during laboratory pain testing. Testosterone therapy also improved some aspects of quality of life.
“If larger studies confirm these findings, testosterone therapy in this patient population may be beneficial in improving pain perception,” Basaria said.
The study included 84 men ages 18-64 years old with opioid-induced testosterone deficiency. Their average age was 49 years. Of this group, 65 participants completed the study. Investigators randomly assigned participants to receive either testosterone gel, applied to the skin, or placebo, for 14 weeks. Thirty-six men received the testosterone gel, and 29 received a placebo.
At the beginning of the study, and then again at 14 weeks, the investigators assessed pain measures and quality-of-life parameters.
For more information on our unique Men’s Testosterone and Wellness therapies visit us at http://www.BostonTestosterone.com or http://www.Facebook.com/BostonTestosterone .
“The Greatest Health of Your Life”℠
Boston Testosterone Partners/Core New England
National Testosterone Restoration for Men
Wellness & Preventative Medicine
http://www.BostonTestosterone.com
http://www.facebook.com/bostontestosterone
855-617-MEDS (6337)/781-269-5953CBlaisdell@corenewengland.com
-
Do You Know Your Sex Hormone Status?
Do You Know Your Sex Hormone Status?
Originally Published by Life Extension Magazine
Zach White reports on why SHBG level testing could be the most important test your doctor isn’t giving you.
Experts have long emphasized the importance of maintaining a balanced and robust sex hormone profile as a core anti–aging strategy.
Hundreds of published studies link improper testosterone and estrogen balance (in men and women) with the onset of age–related pathologies such as coronary artery disease, stroke, osteoporosis, and bone fracture.
But in order for you to optimize your sex hormone status, precise and accurate measurement is of paramount importance.
In this article you will learn of a critical blood marker of hormonal balance called sex hormone–binding globulin or SHBG. Newly published studies reveal that the interaction of SHBG with testosterone and estrogen affects overall hormonal balance— yet very few doctors test for it.
As you will read, sex hormone imbalances precipitated by SHBG abnormalities are associated with multiple diseases of aging in both sexes. These include cardiovascular disease (especially in women), cancer, type 2 diabetes, metabolic syndrome, and sleep apnea.
SHBG: The Master Regulator for Testosterone and Estrogen
SHBG is a protein produced primarily in the liver, although the testes, uterus, brain, and placenta also synthesize it. It serves as a transport carrier, shuttling estrogen and testosterone to sex hormone receptors throughout your body.SHBG also safeguards these vital hormones from degrading too rapidly and prevents their clearance from the body.
It thus acts as the master regulator of your sex hormone levels, maintaining the delicate balance between estrogen and testosterone critical to overall health in aging humans.
New evidence further indicates that the SHBG molecule itself plays another key role in the body: conveying essential signals to the heart, the brain, and adipose (fat) tissue that ensure their optimal function. There’s even a special SHBG receptor molecule on cell surfaces that functions much like the ubiquitous vitamin D receptor protein, helping cells communicate with one another. In other words, SHBG itself functions much like a hormone.
Knowing your SHBG levels, along with testoste–rone and estrogen, thus gives you and your doctor a more precise picture of your overall health—and enables you to take preventive measures against life–threatening conditions for which you may be at greater risk.
Aging Humans and Increasing SHBG: An Overlooked Threat
As you age, SHBG levels may steadily rise, even though your production of sex hormones continues to decline. The result? SHGB binds to what few sex hormones you have remaining and reduces their bioavailability to cells in your body.
With elevated SHBG in the blood, too much testosterone may be sequestered and thus functionally unavailable to healthy tissues. Because testing for SHBG is largely overlooked, many older men (and their doctors) may be led to believe through standard testing that they have “normal” total testosterone levels–but since most of it may be bound to elevated levels of SHBG, in actuality they may be testosterone deficient.
Why? Testosterone, like all steroid hormones, is derived from cholesterol, a fat molecule. Fats don’t dissolve in water, so the amount of testosterone floating freely in your bloodstream is small (about 0.5–2% of the total amount). Most of the circulating testosterone in your blood is either bound to the protein albumin or to SHBG.
It is the combination of free and albumin–bound testosterone that ultimately determines your bio–available testosterone status
As a result of imprecise testosterone measurement, aging men may experience signs of feminization as their increased SHBG binds testosterone, preventing testosterone from exerting its effects and leaving estrogen’s physiological impact on the male physiology unchecked. These may include gynecomastia (the development of fatty breast tissue in men), diminished libido and poor sexual performance, cognitive decline, and chronic fatigue.
Combating Metabolic Syndrome
While excess SHBG creates problems with sex hormone balance, having SHBG levels that are too low is associated with other disorders. Nowhere is the impact of low SHBG so profound as in the cluster of conditions known as the metabolic syndrome, which encompasses obesity, insulin resistance, lipid abnormalities, and chronic high blood pressure.
In men, low total testosterone and low SHBG are predictors for a higher incidence of metabolic syndrome and many of its components.
In late postmenopausal women, low SHBG and high estrogen levels correlate with the inflammatory state associated with metabolic syndrome. SHBG abnormalities have also been linked to an increased risk of acne, infertility, polycystic ovary syndrome, and uterine cancer in overweight women
The high insulin levels found in people stricken with metabolic syndrome have also been shown to suppress SHBG, creating a vicious cycle of abnormal SHBG activity.
The good news is that testosterone supplementation for men, and bioidentical hormone replacement for women, may safely and effectively reverse many of these adverse, age–related metabolic changes. Obtaining accurate measurement of sex hormone levels through SHBG blood testing thus enables you and your doctor to prevent or combat common medical disorders.
Low SHBG Is a Key Marker of Cardiovascular Disease
SHBG levels have an important relationship with nearly every biomarker of cardiovascular disease, from C–reactive protein (CRP) to arterial calcification. Low SHBG is also associated with elevated triglycerides and low–density lipoprotein (LDL).
Calcification of blood vessels, an early finding in cardiovascular disease, is also associated with lower SHBG levels, especially in women. Low SHBG in women is associated with higher levels of C–reactive protein (CRP), an important marker of inflammation and cardiovascular risk. In men, low SHBG indicated an increased risk of death from cardiovascular disease. In both men and women, low SHBG levels are strongly correlated with obesity.
SHBG, alone and in the context of specific sex hormone levels, thus constitutes an integral predictor of a major chronic age–related condition. Some experts are now recommending SHBG measurements as another means of evaluating cardiovascular and metabolic risk.
WHAT YOU NEED TO KNOW: SEX HORMONE-BINDING GLOBULIN • Optimal sex hormone status, including a healthy balance of testosterone and estrogen, is a core component of any anti-aging strategy. • New scientific evidence has revealed the crucial importance to hormone balance of a widely overlooked active protein called sex hormone-binding globulin or SHBG.
• SHBG is an important regulator of your testosterone and estrogen levels, responsible for distributing sex hormones throughout your body—yet few doctors test for it.
• SHBG abnormalities are associated with multiple killer diseases of aging in both sexes, including cardiovascular disease (especially in women), cancer, type 2 diabetes, metabolic syndrome, sleep apnea, and osteoporosis.
Protection from Cancer
Many kinds of cancers of the breast and prostate are stimulated by the sex hormones estrogen and testosterone. However, SHBG interpretations differ for men and women, which is why the SHBG test requires professional interpretation for accurate application.
For example, in human breast cancer cells, higher levels of SHBG inhibit cell proliferation and promote programmed cancer cell death (apoptosis), by blocking the estrogen–related survival mechanisms that most breast cancer cells exploit.
For men, it is the opposite. Higher SHBG levels predict more severe and invasive tumor growth in men with prostate cancer. The association is so strong that some urologists have suggested using SHBG levels as a standard pre–operative measurement to identify patients at high risk of invasive cancers who should undergo a more aggressive surgical procedure.
Optimizing Bone Health
It has long been known that declining estrogen levels in both sexes are significant contributors to bone mineral loss with aging. Experts now recognize that the steady rise in SHBG with aging is directly correlated with bone loss and osteoporosis in both men and women. As a general rule the higher the SHBG level, the less estrogen is available to contribute favorably to bone health.
New studies, however, are finding a direct role for SHBG and its cell surface receptor in bone loss. That suggests an effect that may be independent of estrogen levels. The association is so strong that some experts are now suggesting routine measurement of SHBG as a useful new marker for predicting severity of osteoporosis.
UNDERSTANDING SEX HORMONE LEVELS The terminology for the different measurements of sex hormones in your blood can be confusing, but it needn’t be. Here’s a simple way to think about the levels, using testosterone as an example: Total Testosterone (T) is just that—a measurement of all of the testosterone in a given blood sample. It includes free T, T bound to SHBG, and T bound to albumin.
Free Testosterone is equally simple in concept, though harder to measure. Free T is that small proportion (0.5-3%) of testosterone not bound to SHBG or to albumin.
Bioavailable Testosterone (bioT) is simply the combination of the small amount of free T, plus the much larger amount of T that is loosely bound to albumin. You can also think about bioT as the amount of T that is not bound to SHBG, and some scientists refer to it that way. In general, higher SHBG will mean there’s less T that is bioavailable, while lower SHBG means there’s more bioavailable T, though that is a bit of an oversimplification.
The test for SHBG is useful for understanding and optimizing your sex hormone levels in combination with your other test results.
Detecting Obstructive Sleep Apnea
Sex hormone–binding globulin may provide an important clue that an individual is affected by obstructive sleep apnea, a relatively common condition that increases the risk of heart disease and stroke.
Obstructive sleep apnea occurs when breathing repeatedly stops and starts during sleep due to blockage of the upper air passages. Frighteningly, many people are unaware that they suffer from this disorder. Sleep apnea often manifests with loud snoring, waking up feeling unrested, morning headaches, daytime sleepiness, fatigue, and unexplained high blood pressure. An overnight sleep study (polysomnography) is essential in order to definitively diagnose the condition.
Scientists have found that obstructive sleep apnea is associated with disruptions in the endocrine system in men, including decreased levels of SHBG as well as free and total testosterone. Lower levels of SHBG, free testosterone, and total testosterone correlate with more severe sleep apnea. In one study, men’s SHBG and total testosterone rose significantly following 3 months of sleep apnea treatment with continuous positive airway pressure (CPAP).
Low SHBG combined with low testosterone may represent a novel marker for sleep apnea in men and may provide helpful information regarding which individuals should consider having a sleep study to diagnose the condition.
Summary
Maintaining optimal sex hormone status, including a healthy balance of testosterone and estrogen, is a core component of any anti–aging strategy. New scientific evidence has revealed the crucial importance to hormone balance of a widely overlooked active protein called sex hormone–binding globulin or SHBG. It is an important regulator of your testosterone and estrogen levels, responsible for distributing sex hormones throughout your body—yet few doctors test for it.
SHBG abnormalities are associated with multiple killer diseases of aging in both sexes, including cardiovascular disease (especially in women), cancer, type 2 diabetes, metabolic syndrome, sleep apnea, and osteoporosis.
Like us on Facebook for health tips. http://www.facebook.com/bostontestosterone
cblaisdell@corenewengland.com
781-269-5953
-
Finger Length and The Casanova Pattern – Boston Testosterone Partners
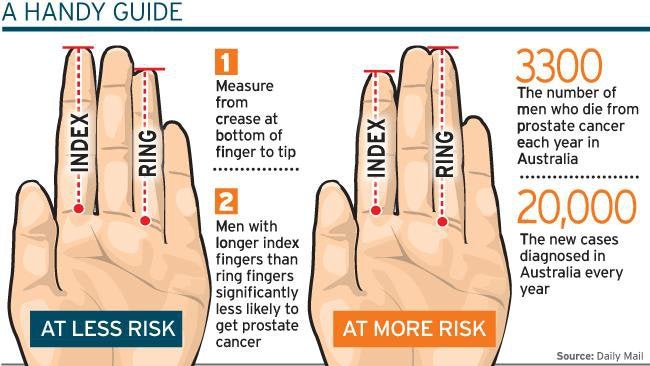
It’s a simple do-it-yourself health test, no equipment needed: Stretch your hands out in front of you and look at how long your fingers are. Most men have ring fingers that are slightly longer than their index fingers, while in most women these fingers are roughly the same length.
So what? Well, variations to these typical findings may have important implications for your health. It turns out that hormones released in the womb influence finger length and, as odd as it sounds, they also have important effects on future health and behavior. Gad Saad, PhD, professor of marketing and research chair in evolutionary behavioral sciences and Darwinian consumption at Concordia University in Montreal, and his colleagues have examined numerous studies involving finger length and found lots of interesting associations.
THE “CASANOVA PATTERN”
Dr. Saad refers to finger length as “a proxy of prenatal testosterone exposure,” explaining that the ratio between the index and the ring finger is determined early in pregnancy. The more exposure the fetus has to this predominantly male hormone, the more so-called masculine traits the adult will have (whether male or female) and the longer the ring finger will be.
Interesting fact: Having a long ring finger is known as the “Casanova pattern,” since Casanova was notably reputed to have a very long ring finger (in relation to his index finger). Dr. Saad told me that this means that “he had a highly masculinized digit ratio.”
According to Dr. Saad, early exposure to testosterone also affects how organs are formed, which is why this ratio is relevant to your future susceptibility to disease. In most people, the discrepancy between the ring and index finger is more pronounced on the right hand than the left.
FINGER LENGTH POINTS TO YOUR FUTURE
Here are some of the conclusions scientists have reached in recent years…
- An impact on disease risk. In the British Journal of Cancer , researchers reported that men whose index fingers were longer than their ring fingers (indicating less prenatal exposure to testosterone) were at lower risk for prostate cancer. On the other hand, scientists at Liverpool University observed that males with longer index fingers were at a higher risk for heart attack than other males, presumably because testosterone is heart-protective.
- A clue to sexuality. The Casanova pattern may offer a clue to sexual orientation. UC Berkeley scientists found that lesbian women tended (like men) to have longer ring fingers than index fingers. But, Dr. Saad said, the findings aren’t so straightforward for gay men. In homosexuals with several older, heterosexual brothers, researchers found a tendency to have much longer ring fingers than straight men… while those without older brothers were more likely to have the same male-pattern, longer ring finger as straight men.
- More sports ability. Scientists believe that high testosterone translates into better success on the playing field, as it encourages aggression, competitiveness and dominant behavior and also facilitates power, endurance and visual-spatial skills. At Temple University, investigators noted that men with longer ring fingers tended to do better in sports such as football and soccer.
- More aggression and risk-taking. At Cambridge University in England, researchers found that financial traders with longer ring fingers tended to be more aggressive and earned the most money. In another study, an analysis of students at Concordia, Dr. Saad and his team discovered that males with longer ring fingers took more recreational, social and financial risks.
LOOKING AHEAD
Your finger length is far from a perfect predictor of your health, of course, but you can consider it a helpful clue to what health challenges the future may hold — so you do all you can to circumvent them. For instance, if you are a male and your finger ratio suggests increased cardiovascular risk, ask your doctor to assess your heart health and pay close attention to cardio-related lifestyle choices such as diet and exercise. Plus, it’s a great conversation-starter when you need to make small talk — and that can be plenty helpful in life, too!
Source: Gad Saad, PhD, professor of marketing, holder of the Concordia University Research Chair in Evolutionary Behavioral Sciences and Darwinian Consumption, John Molson School of Business, Concordia University, Montreal, Quebec, Canada. Dr. Saad is author of The Evolutionary Bases of Consumption (Psychology Press) and the upcoming The Consuming Instinct: What Juicy Burgers, Ferraris, Pornography, and Gift Giving Reveal About Human Nature (Prometheus Books, to be published June 2011). He is a blogger at Psychology Today ( www.PsychologyToday.com/blog/homo-consumericus ).
BOSTON, MASSACHUSETTS – BOSTON TESTOSTERONE PARTNERS/CORE NEW ENGLAND
Testosterone Replacement Therapy with Boston Testosterone Partners , now available nationwide. We are New England’s leading choice for Male Wellness and Hormone Restoration for the treatment Low T, hypogonadism, Andropause and ED. Our medical director is a 25 year MD who has, for over ten years, been balancing both male and female hormones. He has been trained as a Hormone Specialist and has balanced well over a thousand male and female patients across the nation. Our patients have constant doctor interaction, he is always available daily to answer questions for our patients.
Our protocols include Sermorelin-GHRP2 Therapy, Glutathione Therapy, numerous Amino Acid Injectable combinations, personally tailored Weight Loss injectables, Cialis or Viagra sublinguals, Oxytocin sprays, and more..
Our services also include proven medical weight loss systems for BOTH men and women utilizing a proprietary combination of B12, B3, MIC, Amino Acids and L-Carnitine specially compounded for our patients. We offer uniquely compounded SuperB and LipoC injectables and capsules, available only from our compounding pharmacy.
And, we offer TESTOSTERONE REPLACEMENT THERAPY FOR MEN with the THE LOWEST PRICES in the nation!
-
Oxytocin therapy now available at Boston Testosterone/Core New England
Find out about the amazing benefits of Oxytocin Therapy at Boston Testosterone Partners/Core New England .
Oxytocin – the natural way to enhance orgasm in men and women
Known as a desire hormone, the hormone oxytocin is naturally produced in our body and released at key moments – namely when we’re intimate with others. By supplementing this life-enriching hormone, greater orgasm can be achieved far more easily in men and women. Not only this, but oxytocin works to promote a generally improved sense of wellbeing and acts to reduce stress.
The full benefits of oxytocin are only now becoming apparent. It’s involved in the pleasure aspect of sex and is now believed by experts to actually cause orgasm. Studies have found that by supplementing the hormone oxytocin, multiple orgasms can be achieved in women and increased feelings of intimacy can be experienced by both sexes.
Oxytocin hormone supplement the closest thing to a Love Drug
The Oxytocin drug is a safe and potent supplement based on the naturally occurring hormone Oxytocin. It has far reaching benefits for the body and mind, including the ability to enhance orgasm experiences. Oxytocin for men assists emotional bonding as well as desire, and an Oxytocin orgasm for women is especially enhanced.
The hormone Oxytocin is probably best known for its role in childbirth and breastfeeding, although research has established that the Oxytocin drug can help forge deep connections with our partners, our children, our friends and even our pets. Excitingly, the Oxytocin orgasm is powerful for both men and women. It’s been shown to enhance orgasm – and induce multiple orgasms in women.
Oxytocin however, is more than merely a male or female orgasm enhancer. It plays many roles for men, and in women is an essential hormone released throughout their lives in certain conditions and scenarios.
How Oxytocin Hormone is Naturally Released in Body
Oxytocin is produced by the hypothalamus – the almond sized region of the brain located close to the brain stem that links the nervous system to the endocrine system via the pituitary gland. It’s released either via the pituitary gland straight into the bloodstream or to other parts of the brain and the spinal cord.
In childbirth, Oxytocin plays a vital role in triggering and regulating uterine contractions. If the contractions aren’t substantial enough, in a lot of cases Oxytocin is administered to help stimulate these contractions. Not only does this have a physical effect, but Oxytocin is a known as a ‘bonding hormone’ – ensuring that the mother starts to care for her young the moment after giving birth. The emotional and maternal reaction is heightened by the hormone, and the effects establish a bond between mother and baby.
Oxytocin also features in breast feeding. By helping the mother to relax, it allows milk to flow to feed her baby. Through this, scientists and doctors started to take note, as the relaxing and wellbeing effects became apparent.
Research also revealed that Oxytocin plays a huge role in the non-procreative aspects of sex. Both women and men release the Oxytocin hormone during lovemaking – and not only during orgasm. It also appears to be responsible for causing orgasms in the first place.
The Effects of the Hormone Oxytocin in Love Making
At our body’s normal level of production, Oxytocin encourages a mild desire to be kissed and cuddled by your lover. In fact being touched anywhere on the body leads to a rise in Oxytocin levels. This causes a chain reaction within the body, including the release of endorphins and testosterone, which results in both biological and psychological arousal.
Erogenous zones including earlobes, neck and genitals become sensitized to the effect of the hormone, and the body and mind become receptive and proactive in sexual activity. It not only arouses blood and the senses, but also promotes a bond of intimacy and closeness. The cycle continues to fire these pleasure giving endorphins and hormones and we naturally produce more Oxytocin and feel more pleasure as a reward.
By stimulating genital areas and causing the nerves to fire spontaneously, orgasm is reached far easier and more powerfully. In orgasm, male Oxytocin levels quintuple, while women need higher levels if they are to reach orgasm. And during peak sexual arousal, the Oxytocin levels become very high indeed. At this point multiple orgasms can occur.
Oxytocin’s further health and well being benefits
Using Oxytocin can also help regulate sleep patterns, and have a calming effect. Research is ongoing but observation seems to cite Oxytocin’s health giving benefits lying in its ability to counteract stress and the effects of the stress hormone cortisol. Nearly every disease and condition is aggravated by stress; anything that can help counteract the stress is therefore useful.
Oxytocin has a clear physical and emotional power. Not only does the hormone increase orgasm in men and women, it has the natural ability to generate meaningful bonds, calm and in turn increase personal wellbeing.
Prescription Oxytocin nasal spray
We are excited to announce that Oxytocin Nasal Spray is BTP’s latest addition to its comprehensive range of BIO-IDENTICAL HORMONE and TESTOSTERONE REPLACEMENT THERAPY .
Oxytocin is released via the pituitary hormone and it has been clinically proven to have a number of beneficial effects. Oxytocin is being used for mood swings (depression), drug addition, autism, anxiety, schizophrenia, pain (particularly for fibromyalgia) and even as an aid to weight loss, (principally through appetite reduction); but perhaps oxytocin’s most highlighted use has been to help couples enjoy a closer (bonding/ loving) relationships and for individuals, (in particular for women- which in this case is unusual) to have more intense orgasms.
The world’s expert talks about this calming hormone
An Interview with Kerstin Uväs-Moberg, M.D., Ph. D
If you suffer from stress, high blood pressure, elevated cortisol in the blood, or other stress-related symptoms, you will be interested in oxytocin—a hormone which Dr. Kerstin Uväs-Moberg calls the calm and connection hormone.
How can you bring greater calm and connection into your life and the life of your children?
Kerstin Uväs-Moberg, M.D., Ph. D, author of The Oxytocin Factor, is a recognized world authority on oxytocin. Her research took place at the famed Karolinska Institute in Stockholm and at the Swedish University of Agricultural Sciences in Uppsala, where she is Professor of Physiology. Influential in obstetrics, psychology, pediatrics, child development, physical therapy and other fields, Dr. Uväs-Moberg has authored over four hundred scientific papers and lectures widely in Europe and the USA.
1. In your book, you state, “There are many scientific conferences on the topics of stress and pain, but very few conferences deal with calm, rest, and wellbeing.” What does oxytocin have to do with calm, rest, and wellbeing?
Dr. Uväs-Moberg: Oxytocin, which was first noticed during birth labor and in nursing
mothers in 1906, acts as both a hormone and a neuropeptide. It triggers a complex series of reactions that enhance your body’s relaxation and calmness. This is important in two ways. The first (1) is the immediate health benefit of lowering stress-related symptoms and the second (2) is that repeated dosages of oxytocin seem to convert the immediate benefit into a long-lasting effect. In our studies, animals who received as little as one dose per day for 5 days needed little additional oxytocin to stay calm for up to 3 weeks. This suggests that oxytocin can offer stressed human beings a way to open up new pathways, to help them relax and restore calm immediately and across long term situations. I stress oxytocin’s ability to grow or develop people’s relaxation and restoration capacity.
2. What is the relationship between oxytocin and adrenaline or other fight/flight responses?
Dr. Uväs-Moberg: The body is intelligent. Oxytocin does have the reverse effects to flight or fight hormones, but the body doesn’t call on oxytocin in every situation. Sometimes we are threatened or in danger and we must respond to our flight or fight hormones to protect ourselves. However, oxytocin may even be able to serve us in potentially threatening situations. For example, if we can stay calm in a tense situation, we may know enough to move away from danger. We can learn to avoid a fight and respond differently.
3. What does oxytocin actually do?
Dr. Uväs-Moberg: Oxytocin does two important things: (1) lowers blood pressure and other stress-related responses, and (2) increases positive social behaviors, such as friendliness and desire to connect. Oxytocin impacts the body in two ways. The first is that it is a hormone released from the blood stream as it circulates in the body. And, it is also released by the nerve centers inside the brain. This means that it capable of having a direct impact because it is not only a blood born hormone.
Today, in my opinion, our relaxation responses are under-developed and we are much more stressed than we have been historically. Therefore, everything that we can do to enhance our levels of oxytocin increases our options for wellbeing. The results of an interesting longitudinal study between mothers and children demonstrate that real contact (eye contact and direct conversation) between mothers and children has been reduced by half. Mothers and their children are spending time in the same room, but only about half that time is spent in real contact. Our stress may be passed on to the children in this way.
4. Are there ways that people can increase their oxytocin levels in daily life?
Dr. Uväs-Moberg: Although some are thinking about developing oxytocin drugs, I believe the absolute best thing to do is to activate your own oxytocin. Your body knows how to handle that oxytocin. There are several things that anyone can do:
Touch is very important. Interactive touch with human beings is best, but it doesn’t have to be limited to human beings. Touch happens between people and their pets.
Getting massage is helpful.
Walking, swimming in warm water, and all physical exercise is excellent.
Deep interaction, intimacy, and eye-contact are also important.
Sex releases oxytocin.
Safety is important. For example, nursing mothers exhibit behavior associated with oxytocin when they are in a calming, familiar room. If you move them to an unknown and more stressful environment, their safety levels fall and so do their oxytocin behaviors. Therefore, in the latter case, their capacity to bond with their babies is reduced. In another example, studies have shown that small groups, 6 – 10 people, seem to have a positive impact on cardiovascular and cancer patience. This may be because oxytocin is released in the safety of these settings. Perhaps we need to make sure our family settings include levels of intimacy rather than just spending time in the same house. Maybe our economic success, which affords us the ability to sleep in separate rooms and/or beds, has actually deprived us of the touch necessary for future success in calmness, connection, and intimacy. When people had less money, children had to sleep together in the same beds or listen to night time stories rather than play individual computer games. Societies at that time had built in bonding and companionship mechanisms. We need ways to restore these to our children.
5. Oxytocin is often thought of as a female hormone. Do men have oxytocin and, if so, how does it operate in their lives?
Dr. Uväs-Moberg: Both men and women have oxytocin and in almost the same amount. Pregnancy, labor, and nursing activate oxytocin in women and, obviously men do not have the same activation. But men appear to experience oxytocin when they relate to their children and they also experience oxytocin with touch. It is both a mistake to say that oxytocin is only a female hormone and not a mistake because we do not know all the ways that oxytocin is activated in men.
6. Your research has supported the ‘Peaceful Touch’ programs in Swedish public schools. What is ‘Peaceful Touch’ and what results have been reported by the school systems?
Dr. Uväs-Moberg: ‘Peaceful Touch’ is a program that works in a variety of ways. One of the most important is that children are taught how to touch each other in peaceful ways. Discipline problems have become very common in Swedish schools. Teachers report that Peaceful Touch programs have (a) reduced the level of aggression in the classroom, (b) increased the length of time students can sit still, (c) enhanced students’ ability to listen, and (d) improved their ability to take information in. It is important to realize that massage and/or peaceful touch is beneficial to both the giver and the receiver. This activity is much better than giving children drugs to control their behavior. There should be more money for good research of these programs in Swedish schools. Oxytocin research also suggests that parents and children learning to give each other ‘Peaceful Touch’ could be very beneficial. I recognize that ‘touch’ is a very controversial issue now, but believe that we may be able to find ways, even if it isn’t physical touch, to give our children experiences with calm and connection.
7. Are there any medical conditions that you think might be helped by oxytocin?
Dr. Uväs-Moberg: Children like autistic children, or others who have problems opening up, could benefit from oxytocin. But, before we start talking about medical use of oxytocin, I believe we need a new system of ethics. Unlike other ‘feel good’ drugs, oxytocin is very subtle. People might not even realize that they’ve taken oxytocin. An interesting study reported in the June 2005 issue of Nature examined the role of interpersonal trust and oxytocin. Ernst Fehr of the University of Zurich and his colleagues discovered that men who inhaled a nasal spray spiked with oxytocin gave more money to partners in a risky investment game than did the men who sniffed a spray with no active ingredient. The researchers concluded that “oxytocin specifically affects an individual’s willingness to accept social risks arising through interpersonal interactions.”
Can you imagine this happening without people knowing they have been exposed to oxytocin? A good thing could be used for bad purposes. Obviously, it will be wonderful if we can help autistic children and others who cannot open to interpersonal relationships, but we need to think deeply about the ethics involved in any larger use.
8. Do you believe that there is relationship between intuition and oxytocin?
Dr. Uväs-Moberg: Yes. Oxytocin fosters openness. I am convinced that intuition is one branch of that opening. For example, nursing mothers report a profound connection with their children and often intuitively know what their babies want, although the babies can’t express themselves verbally. I believe that this knowing is an intuitive process. There are many interesting questions about how intuition might work. For example, what is the difference between memories and images which seem to arise from the future? How can we keep intuitive images clear and not distorted by wishful thinking or psychological reactions? These are interesting questions which should be explored someday.
9. Assuming that you could do any further research on oxytocin that you wanted, what would interest you?
Dr. Uväs-Moberg: Two of the most interesting frontiers in oxytocin research are (1) the mental, mind, or psychological state of a person and (2) the relationship between spirituality and oxytocin. In the former, I am interested to know if seeing images or thinking about things that relax you also causes the release of oxytocin. The neuroscientist and author, Antonio Damasio of Iowa University, raised this issue in an editorial in the same June 2005 Nature. When asked if he thought that crowds of shoppers might be persuaded to purchase more if they were sprayed with oxytocin, Damasio referred to slick marketing campaigns that people are already exposed to. He said that these campaigns lure, ‘you in with images of wonderful landscapes or sex, and [they] probably work in exactly the same way.” I, too, suspect that this images release oxytocin, but research needs to be done on how oxytocin works with mind or mental states.
In the case of spirituality, it may be that prayer, contemplation, and meditation also activate oxytocin, but we have no way of knowing. Energy medicine professionals are searching for ways to measure the physiology of body energy. To date, I do not know of any reliable way to do this, but I believe that oxytocin will play a role and that common principles may be found in the Body/Mind/Spirit interaction.
-
MEN RECEIVING TESTOSTERONE REPLACEMENT THERAPY HAVE LOWER RISK OF CANCER, CONFIRMS STUDY
A large study that took place over nearly nine years has concluded that men receiving testosterone replacement therapy have a lower risk of cancer than those not receiving, or balancing, their hormones. The study confirmed that there is no increased risk of cancer while on TRT, including prostate cancer .
This is something that many testosterone doctors have known for years but the myth has continued to propagate nonetheless.
“Men have been so concerned about the relationship between testosterone and prostate cancer development so it’s refreshing, finally, to have a solid clinical answer that there is no relationship between the two,” said Charles Blaisdell, Clinic Director at Boston Testosterone Partners, a center specializing in the treatment of Low Testosterone in men.
The study that was conducted took place that the Baylor College of Medicine in Houston by Dr. Michael L. Eisenberg and his associates. It began by evaluating their database of men who had a baseline serum testosterone level. Of those men, they then documented those who were on testosterone replacement therapy. The study’s participants included 750 men who resided in Texas. The study went on to link the records of these men to the Texas Cancer Registry to confirm or deny the incidence of cancer in all 750.
Out of the 750 men chosen for the study 333 of them were on testosterone replacement therapy and 417 of them were not. The average age of the male participants was 47 years and the mean time frame that they were studied was 8.7 years.
“The study is important for aging men with untreated low testosterone ,” says Blaisdell. “Of the 750 men in the study a total of 55 of the men had developed some form of cancer in the almost 9 years. But, importantly, of the 55, only 22 of the men were on those on testosterone replacement therapy while the other 33 were the men who were not receiving the benefits of testosterone replacement therapy,” he went on.
“These researchers even went as far as to adjust the age and years of therapy; they still found no difference in the risk of developing cancer of the men undergoing testosterone replacement therapy,” Blaisdell said.
When compared to the general Texas population, men on testosterone replacement therapy had an age-adjusted standardized cancer incident rate of 1.5 while those who were not on testosterone replacement therapy had a standardized cancer incident rate of 1.7.
The men who were not undergoing testosterone therapy had a much higher rate of cancer. Blaisdell postulates, “This is simply because men who treat their hormone deficiencies have multi levels of health protections. First, they are perfectly optimizing their testosterone and hormone levels so their hormonal health is second to none. Next, men who undertake TRT, generally will care for themselves in all other aspects of health. Regular physical exercise, mental exercise such as yoga or meditation and clean diets are commonplace among all our patients. Men with perfectly optimized hormones do not sit on the couch with a beer and a bag of chips in each hand”
These researchers also undertook to analyze the incidents of prostate cancer. As to that risk, the researchers discovered that men on testosterone replacement had an age adjusted standardized cancer incident rate of 2.6 versus a higher standardized cancer incident rate of 3.7 of men who were not on testosterone replacement therapy.
“We had hoped for these results,” Dr. Eisenberg said during a session at the annual meeting of the American Urological Association. “Certainly people are worried about testosterone in terms of prostate cancer development.”
-This is not the first study to conclude that Testosterone Replacement Therapy has been reducing the risk in prostate cancer in men. In a study reported this year also, Stanford researchers compared data of 722 men as well as the general population and concluded there was a decrease in prostate cancer incidence among those treating themselves with medical testosterone therapy. (The Journal of Urology, Volume 189, Issue 4, Supplement , Pages e617-e618, April 2013.)
Testosterone therapy also plays a big role in lengthening the life span of men.
“Today, we recognize, based on dozens of studies, its importance relative to health issues such as diabetes, obesity, metabolic syndrome, and osteoporosis,” says Boston Testosterone Doctor, Abraham Morgentaler. “Men with low T die sooner than men with normal levels of testosterone,” says Morgentaler, Harvard Doctor and author of the leading men’s health book Testosterone for Life: Recharge Your Vitality, Sex Drive, Muscle Mass, and Overall Health .
Boston Testosterone Partners is uniquely positioned to conduct testing for Low Testosterone for men nationwide. If you are interested in having yourself checked for Low T you may contact Charles Blaisdell at cblaisdell@corenewengland.com or 617-869-7961.
Boston Testosterone Partners /Core New England is a Testosterone Replacement, Wellness and Preventative Medicine Medical Center that treats and prevents the signs and symptoms associated with Andropause and hormone imbalances. With affiliates nationally, BTP offers hormone replacement therapy, weight loss protocols, erectile dysfunction (ED), Sermorelin-GHRP2 therapy and neutraceutical injectable therapies for men and women. Their medical facilities offer physician examinations and treatment programs that incorporate the latest in medical science. For more information, reviews and testimonials go to their Facebook Wall or call 855-617–MEDS (6337)/781-269-5953.
-
The Simple Diet
Confused about what to eat? Here is a great Simple Diet from T Nation.
The Simple Diet
by Tim Henriques – 3/28/2012 – T-Nation
Science can make nutrition complicated. Measure the glycemic index of this, the glycemic load of that. How much omega-6’s in this? What about omega-3’s?
While a deeper level of nutrition knowledge can certainly be useful, what we often get through the media are little bits of information that’s never paired with an overall philosophy.
It becomes especially hard when faced with nutritional science that seems to contradict itself. Eggs are a great source of protein and healthy fats. No, eggs have too much cholesterol and “bad” saturated fat. What do we do?
Enough. Here’s my philosophy: I call it the Simple Diet, because it’s simple to understand and the foods you’re eating will be in their simple, or basic, form.
This diet is particularly useful when you want to lean up a bit but still live a relatively normal lifestyle. If you hope to get unbelievably cut or prep for a bodybuilding show, this likely isn’t for you, but if you found that your holiday bingeing has extended into spring training, then this might be your answer.
This diet assumes you’re working out reasonably hard at least several days a week. If you’re not doing that, start. If you don’t plan on doing that, you’re on the wrong website.
Builders & Energy Providers
I think of food in terms of two categories: builders and energy providers. That’s how I teach the nutrition basics to my kids, who are all five and under. It’s simple, and it works. You can also add a third category: stuff that keeps you healthy.
This paradigm matches nicely with the primary functions of nutrients, which are to provide energy, build and repair tissue, and regulate metabolism.
Builders. The meathead’s favorite food group. The stuff that does this job is protein and fat. On this diet, you can eat as much natural, unprocessed protein and fat as you want.
Here are some examples:
Red meat
Eggs (whites or whole)
Chicken (with/without the skin)
Turkey (with/without the skin)
Fish (with/without the skin)
Butter
Coconut oil
Olive oil
You’ll notice that I’m pushing unprocessed foods. Slicing turkey meat from an actual turkey breast is better than opening a package of pressed mechanically separated turkey parts. You already know this, because that turkey sandwich the day after Thanksgiving tastes a hell of a lot better than that five-dollar foot long from Subway, it’s just less convenient. Get over it.I’m a big fish fan. One of the rules of this diet is that you have to eat fish at least twice a week, and the more the merrier. However, fish from a can doesn’t count – it’s not off-limits, but it doesn’t count toward your twice-a-week total. Non-farmed fish is ideal, but work with what you have access to.
I’m not as excited about pork. Fish and lean red meat (and wild game if you have access to it) is number one. Pigs aren’t as good, in my opinion. Sneaking in some lean pork tenderloin is permitted, but no bacon or hot dogs. They’re processed junk.
Avoid things like mayonnaise, peanut butter, and sour cream. Mayo is too processed and peanut butter and sour cream, while natural, are better for weight gain, and this is a weight loss program. If you find yourself losing weight too fast and aren’t trying to get ultra lean, you can add those foods back in.
Energy providers. This is where carbs fall. This is not a low-carb diet – those diets can work but can be a pain to follow, not to mention they cause intense workouts to suck. This diet will have carbs, but they’ll be of the healthy sort.
Here’s what you can eat:
Potatoes (any version in its natural state)
Sweet potatoes (ideal)
Rice (any version)
Oatmeal (any version but steel cut preferred)
Any fruit
Any veggie
Note: Wraps and the like may be used sparingly (once or twice a week)You may have unlimited amounts of any of the foods from either of the above categories. Yes, unlimited. Most people don’t crave natural foods, and there are far fewer reports of binging on chicken and rice than beer and wings. Natural foods are also enormously satisfying and contain more fiber, so they fill you up quicker.
Natural foods are also much harder to come by. You can get junk food at 2 AM just by hitting up the drive thru or vending machine. You’re much less likely to have a post-bar binge-fest if it requires grilling up chicken and digging out the rice cooker.
Finally, natural foods tend to spoil, so you usually don’t have unlimited quantities lying around, and they’re expensive – so even if your head or stomach doesn’t tell you to stop eating, your wallet will.
You still might find yourself a bit hungry or experiencing cravings while on this diet. That’s expected, but it won’t be cravings for these foods.
Rules
You will have veggies at every meal. Yes, every meal, including breakfast. You can have whatever veggies you want, but fresh or frozen is preferred over canned. Your veggies should be bright and colorful and actually have taste.
Peas, broccoli, shredded peppers, and mixed veggies are my personal favorites, but have whatever you want. This will help you feel full, give you some energy, and along with the good fats, help take care of the third category, keeping you healthy.
Avoid any processed carbs, junk food, desserts, sugar, soda, and fruit juice – all off limits. Pasta and bread are also on the avoid list.
Of course, you can eat that stuff if you must, just be aware that you’re cheating if you do. There are also no diet drinks allowed – no Diet Snapple, Pepsi One, Coke Zero, etc. They’re not natural things so they don’t qualify (hey, it’s my diet!).
Basic rule, if the food doesn’t look pretty close to what came out of the ground, you can’t have it.
Notes
Nuts. While healthy, nuts tend to slow down the weight loss process. If you’re losing weight too fast, or trying to gain a bit of muscle, then by all means include them. But for straight fat loss, go nut-free for a month and see what happens. You can then make a decision based on the results.
Coffee. I’m not a coffee drinker, but if you’re going to drink it in its relatively natural state (meaning your cup of joe doesn’t resemble a 30-ounce milkshake with caramel drizzle), then it’s likely okay. I also don’t think a person should be addicted to anything, so if you go into caffeine withdrawal without coffee, it’s time to get that under control.
Milk. I like milk and tend to include it in my diets. Start off with 16 ounces or less of whole milk (preferably organic) per day and see how you respond. If you’re losing weight too fast, start to add it back in, if not keep it out. The same holds true for most dairy products like yogurt and cottage cheese.
Alcohol. From a health and fitness point of view, wine is the best (although I don’t drink it, much to my wife’s chagrin). Try limiting wine to one or two times a week and see how you respond. I’d avoid beer or hard alcohol, although you can have them with your weekly cheat meal.
My rule of addiction holds true here, too, so if it’d be hard for you to go a month without booze, then now’s the time to stop and get it under control. One of my favorite quotes (from Epictetus) is, “No man is free who is not a master of himself.”
Supplements. While no diet “needs” supplements, a good peri-workout protocol would be one of the first things I’d put back into a diet, especially if you’re going for that “pretty lean but still big and powerful” look. Check out the Anaconda™ Protocol – the feedback is astounding.
Cheating
What I like about this diet is that you can follow it long term. I should point out that to me, a diet doesn’t mean a plan you follow for a set time to accomplish a goal; it’s simply a word to describe one’s eating.
But denying yourself sucks, and we only have so much will power, so I want you to cheat on this plan. For one meal, once a week, every week, you can eat whatever you want, as much as you want. No limits.
Ideally, eat reasonably healthy for that meal; go out to a restaurant and order the fish and rice, but add that appetizer or dessert that you’ve been craving. In other words, it’s better to do “little cheats” instead of a big cheat.
So if you’re craving food not on the plan, eat a healthier choice like spaghetti with meat sauce instead of three Big Macs. Think of food as a continuum; just because you’re cheating doesn’t mean you have to go completely to the other side.
The leaner you are, the closer to where you want to be physique-wise, the more you can cheat. The heavier you are, the further away from your goals, the less you can cheat. You can rationalize this by saying heavier folks have already been cheating so now it’s time to pay up and be strict, while leaner people have earned a bit of freedom with their diet and can enjoy themselves accordingly.
Simple Summary
What to eat
Unlimited natural, unprocessed meat (chicken, turkey, red meat, wild game)
Unlimited animal skin
Unlimited natural fat
Fish (not from a can) twice per week minimum
Veggies with every meal, no exceptions
Unlimited fruit
Unlimited potatoes, sweet potatoes, rice, and oatmeal
If you follow the above rules, one meal per week eat whatever you want, as much as you want.
Note: Choose organic and/or high quality versions of the above foods whenever possible or as budgetary restrictions allow.Maintenance
A typical 200-pound male following this plan should lose 1-2 pounds a week of mainly fat. Use the stomach/waistline as a progress guide – over time it should get smaller and noticeably leaner.
Once you’ve reached your goal you may modify the program a bit. You might include another cheat meal, or simply try to eat another meal on top of what you’re normally consuming to prevent further weight loss. Adding in additional pre or post workout nutrients would be the best place to start. By this point you should have learned how your body responds to different foods and can make changes appropriately.
Get Simplified
What’s great about this diet – apart from its efficacy – is that you can follow it for a long time, it works pretty well with “real life,” and it still supplies enough energy to get through your T Nation approved workouts.
But it isn’t complicated – when it comes to nutrition, simpler is often better.
-
Sermorelin Therapy for Weight Loss and Lean Muscle Mass
What is Sermorelin?
Sermorelin is an analog of Growth Hormone Releasing Hormone (GHRH) that is produced within the human brain and which stimulates the natural production and release of Human Growth Hormone (HGH) by the pituitary gland.
In our younger years, ample amounts of GHRH are produced so that the pituitary is able to provide the body with sufficient growth hormone to sustain health, vitality and vigor.
GHRH declines with age causing reduced production and secretion of pituitary HGH and thereby increasing the probability of growth hormone insufficiency.
Sermorelin a natural product designed replicate the effects of GHRH and act as a trigger to stimulate the body to produce it’s own HGH.
Simply, Sermorelin therapy jump-starts your body’s own production of HGH!
What are the benefits and advantages of Sermorelin?
Human Growth Hormone (HGH) therapy has been used extensively and successfully for many years, and has proven effective for countless patients, worldwide.
Although usually effective and safe, direct injection with HGH is not universally the best approach to treating declining levels of growth hormone in every patient.
Unlike HGH therapy — which directly replaces declining levels of HGH from the outside — Sermorelin attempts to address the primary cause of declining HGH from the inside by naturally stimulating the pituitary gland to produce more HGH.
This natural stimulation of the pituitary is designed to preserve the operation of growth hormone production mechanisms that are declining as we age.
Sermorelin benefits include
• Increases natural production of Human Growth Hormone
• Improves Physical Performance
• Improves Immune Function
• Increases IGF-1
• Improves sleep quality
• Decreases body fat
• Increases lean muscle mass
While Sermorelin produces largely the same effects on body composition, mood and the other benefits of HGH, it also has some additional and important benefits for many patients.
Additional benefits of Sermorelin HGH treatment
• The effects of Sermorelin are naturally regulated at the level of the pituitary gland by negative feedback and by release of somatostatin, so that medical concerns associated with the possibility of HGH overdosing are minimized.
• Tissue exposure to HGH released by the pituitary under the influence of Sermorelin is episodic — not square wave — therefore avoiding the possibility of tachphylaxis by mimicking normal physiology.
• For some patients, Sermorelin has a better overall safety profile, and its use for adult hormone deficiency is not restricted.
• Sermorelin-based HGH treatments are also far less expensive than direct injection of HGH.
Call or email Boston Testosterone Partners for more information on products and pricing.
855-617-MEDS (6337)/781-269-5953
CBlaisdell@corenewengland.com